Schizoaffective disorder vs Schizophrenia: Two mental health conditions that are often mistaken.
And let’s be honest—mental health can be complicated. But understanding it? That’s the key to living a healthier, more fulfilling life.
So, let’s break it down.
Are schizophrenia and schizoaffective disorder the same?
Not quite. While they share some similarities, they’re two distinct mental health disorders with unique symptoms and treatment approaches.
Here’s the deal:
- Schizophrenia affects how someone thinks, feels, and behaves, often involving psychosis.
- Schizoaffective disorder. That’s a mix of schizophrenia symptoms and mood disorder features like depression or mania.
Understanding these differences is crucial—whether you’re seeking clarity after a diagnosis, supporting a loved one, or just curious about mental health.
In this guide, we’ll explore:
- How these disorders are related.
- What makes them different?
- What it’s like to live with them.
When it comes to schizoaffective disorder vs schizophrenia, proper diagnosis and care can make a world of difference.
So, stay tuned as we break down the symptoms, treatment options, and tips for managing both.
Understanding Schizophrenia
What is Schizophrenia?
Schizophrenia is a chronic mental health condition that affects how a person thinks, feels, and behaves. It occurs due to changes in brain structure and function, impacting how information is processed.
Research suggests that certain areas of the brain, like the prefrontal cortex and hippocampus, may be smaller or function differently in people with schizophrenia. These changes can affect memory, decision-making, and emotional regulation.
Imbalances in neurotransmitters such as dopamine and glutamate are also linked to the condition, disrupting how the brain processes signals and potentially altering perceptions and thought patterns.
These differences in brain function can lead to challenges in interpreting reality and managing daily life. However, understanding these changes is key to developing effective treatments and fostering empathy for those living with schizophrenia.
The Schizophrenia Spectrum
As part of the “schizophrenia spectrum”, symptoms can range widely in severity and presentation, often disrupting daily life and relationships.
Common psychotic symptoms include:
- Hallucinations: Hearing or seeing things that aren’t there.
- Delusions: Holding false beliefs despite clear evidence to the contrary.
- Disorganized thinking and speech patterns.
- Social withdrawal.
- Reduced emotional expression or motivation.
According to the DSM-5 criteria, schizophrenia is diagnosed when symptoms persist for at least six months, with at least one month of active-phase symptoms (e.g., hallucinations, delusions, or disorganized speech). Diagnosis also requires significant functional impairment, such as difficulties in work, relationships, or self-care.
Prevalence and Challenges of Schizophrenia
Schizophrenia affects about 1 in 300 people worldwide, making it a relatively uncommon but serious mental health condition. It typically develops in late adolescence or early adulthood, with men often showing symptoms earlier than women. Individuals living with schizophrenia face several challenges, including:
- Stigma and widespread misconceptions about the disorder.
- Limited access to effective mental health care.
- The need for long-term management through medication, therapy, and social support.
Treatment Options for Schizophrenia
Managing schizophrenia often involves a combination of approaches, including:
- Medication: Antipsychotics are the most common medications used to reduce symptoms like hallucinations and delusions.
- Psychotherapy: Cognitive Behavioral Therapy (CBT) can help individuals manage symptoms and develop coping strategies. Here’s more information about CBT.
- Supportive Therapy: Social skills training and vocational rehabilitation provide tools for daily life and work.
- Family Education: Programs that educate families about the disorder can improve support systems.
- Lifestyle Adjustments: Stress management, regular exercise, and healthy routines can enhance overall well-being.
- Community Support Programs: Access to housing, job placement, and peer support groups can improve independence and overall living.
Why Early Intervention Matters
Early diagnosis and treatment are crucial for improving outcomes. Timely intervention can help individuals manage symptoms, enhance daily functioning, and achieve a better quality of life.
What is Schizoaffective Disorder?
Schizoaffective disorder is a complex mental health condition that combines symptoms of schizophrenia. These are hallucinations, delusions, or disorganized thinking, and it’s paired with significant mood disturbances, such as depression or mania.
In essence, it is a “hybrid” disorder. It’s blending features of psychotic disorders and mood disorders, which makes it challenging to diagnose and manage.
Key Diagnostic Criteria:
- Psychotic symptoms (e.g., hallucinations or delusions) must persist for at least two weeks in the absence of mood symptoms. This distinguishes schizoaffective disorder from mood disorders with psychotic features.
- Mood symptoms (e.g., depression or mania) must be present for the majority of the illness’s duration, occurring alongside psychosis.
These diagnostic criteria ensure that schizoaffective disorder is differentiated from schizophrenia and mood disorders.
Types of Schizoaffective Disorder
Schizoaffective disorder is categorized into two distinct types, depending on the nature of the mood symptoms experienced alongside psychosis:
- Bipolar Type: This subtype includes symptoms of mania or a mix of mania and depression in addition to psychotic symptoms. Individuals may experience heightened energy, euphoria, impulsivity, or severe mood swings.
- Depressive Type: This subtype is characterized by major depressive episodes alongside psychotic symptoms. Symptoms may include persistent sadness, hopelessness, fatigue, and a lack of motivation.
The distinction between these types is crucial as it informs the treatment plan, with the bipolar type requiring mood stabilizers or medications for mania, while the depressive type often involves antidepressants.
How Common is Schizoaffective Disorder?
Schizoaffective disorder is relatively rare compared to schizophrenia, with fewer reported cases.
However, its impact on surviving daily can be significant. More often than not, individuals with schizoaffective disorder often face challenges in managing psychotic episodes and mood swings.
The results? Functional impairments in work, relationships, and overall quality of life.
Treatment Options for Schizoaffective Disorder
Treatment for schizoaffective disorder is tailored to address both mood symptoms and psychotic symptoms, typically involving:
- Antipsychotics to manage psychotic symptoms like hallucinations or delusions.
- Mood stabilizers to treat mood disturbances, especially in the bipolar type of schizoaffective disorder.
- Antidepressants for addressing depressive episodes in the depressive type of schizoaffective disorder.
- Psychotherapy, such as cognitive-behavioral therapy (CBT), helps with emotional regulation, coping strategies, and improving overall functioning.
- Supportive care, including social support, vocational rehabilitation, and case management, to assist with daily life challenges and maintain stability.
Unique Challenges
Living with schizoaffective disorder presents the challenge of balancing treatment for both psychotic and mood instability symptoms simultaneously. This dual focus can complicate finding the right therapy or medication, requiring a highly individualized approach.
How Is Schizoaffective Disorder Different from Schizophrenia?
Understanding the difference between schizoaffective disorder and schizophrenia is at the heart of this discussion.
While both conditions share psychotic symptoms, they differ significantly in how they manifest, are diagnosed, and treated.
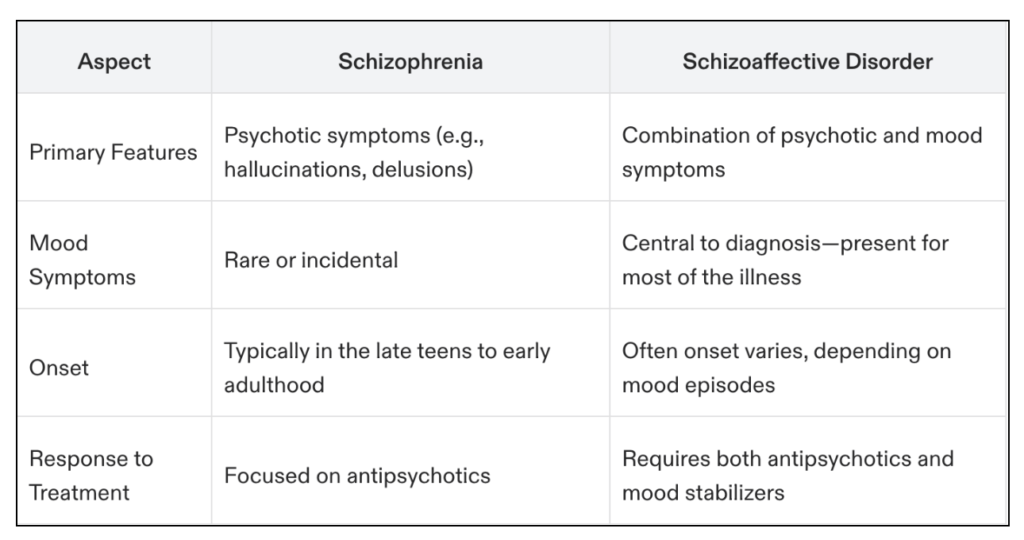
At a glance, we can find their key difference here.
Expert Insights: Let’s see this from a medical expert’s point of view.
- Dr. Emily White, Psychiatrist: “Understanding the nuanced differences between schizophrenia and schizoaffective disorder is crucial for accurate diagnosis and effective treatment planning.”
- Professor Alex Carter, Clinical Psychologist: “Schizoaffective disorder presents a unique challenge due to the overlap of symptoms from both psychotic and mood disorders. Early intervention and integrated treatment strategies are key.”
Let’s dive deeper to explore these distinctions and gain a clearer understanding of these complex mental health conditions.
Schizoaffective Disorder vs Schizophrenia: Key Differences
So how is schizoaffective disorder different from schizophrenia?
We can identify it by looking at their core symptoms, timing/duration, and treatment approach.
Core Symptoms
Schizophrenia: The primary feature of schizophrenia is psychosis, which includes symptoms such as hallucinations, delusions, and disorganized thinking. While individuals with schizophrenia may also experience depression or other mood-related symptoms, these are secondary and not part of the core diagnostic criteria. Schizophrenia primarily affects cognitive and perceptual processes, disrupting a person’s ability to interpret reality.
- Main feature: Psychosis (hallucinations, delusions, disorganized thinking).
Schizoaffective Disorder: In contrast, schizoaffective disorder integrates both psychotic symptoms and prominent mood symptoms as part of its core presentation. These mood symptoms can include episodes of mania, hypomania, or depression. The duality of mood and psychotic disturbances makes schizoaffective disorder a blend of schizophrenia and mood disorders like bipolar disorder or major depressive disorder.
- Schizoaffective Disorder at a Glance: Characterized by a combination of psychotic symptoms (like hallucinations or delusions) and significant mood episodes (mania, hypomania, or depression), blending features of schizophrenia and mood disorders.
Duration and Timing of Psychosis
Schizophrenia: Psychotic symptoms are persistent and not tied to mood episodes, meaning they occur independently of any mood changes. Symptoms such as hallucinations and delusions are consistently present over time. To meet the diagnostic criteria for schizophrenia, these symptoms must persist for at least six months, with active psychotic episodes lasting for at least one month. The timing and duration of these symptoms are key in distinguishing schizophrenia from other conditions, as the disorder involves ongoing disruptions in thought, perception, and functioning that extend well beyond temporary episodes.
- Duration and timing: Symptoms must persist for at least 6 months, with active psychotic episodes lasting at least 1 month.
Schizoaffective Disorder: For a diagnosis of schizoaffective disorder, psychotic symptoms must occur independently of mood disturbances for at least two weeks. This is a key diagnostic distinction, as psychosis in schizoaffective disorder is not exclusively tied to episodes of mania or depression. Instead, it exists as a separate feature, independent of mood fluctuations.
- Schizoaffective Disorder: Psychotic symptoms must occur on their own, without mood disturbances, for at least two weeks.
Treatment Approach
We mentioned earlier that effective treatment for both schizophrenia and schizoaffective disorder requires a comprehensive and personalized approach, as these conditions manifest differently in each individual.
Schizophrenia: The cornerstone of treatment for schizophrenia is antipsychotic medications, which help reduce or eliminate symptoms like hallucinations, delusions, and disorganized thinking.
Schizophrenia Treatment:
- Medications: Primarily treated with antipsychotics to reduce symptoms like hallucinations, delusions, and disorganized thinking.
- Therapy: Cognitive Behavioral Therapy (CBT) helps with coping strategies, communication skills, and symptom management.
- Psychosocial Interventions: Vocational training, family support programs, and social reintegration strategies.
Schizoaffective Disorder: Since schizoaffective disorder includes symptoms of both schizophrenia and mood disorders, its treatment often involves a combination of approaches. Antipsychotic medications target schizophrenia-like symptoms, while mood stabilizers or antidepressants are prescribed to address mood swings or depressive episodes.
Schizoaffective Disorder Treatment:
- Medications: Combines antipsychotics (for schizophrenia-like symptoms) with mood stabilizers or antidepressants to address mood swings or depressive episodes.
- Therapy: Focuses on emotional well-being, managing symptoms, and improving overall functionality.
The Importance of Personalized Treatment Plans
Both disorders require treatment plans tailored to the individual’s specific symptoms, needs, and circumstances. Regular monitoring and adjustments are essential, as responses to medications and therapies can vary greatly. A multidisciplinary approach involving psychiatrists, therapists, social workers, and support networks offers the best chance for long-term stability and improved quality of life.
Schizoaffective Disorder vs Schizophrenia Prognosis
Schizophrenia: Schizophrenia often requires lifelong management. Functional recovery varies, with some individuals responding well to treatment while others face persistent challenges in daily living and social interactions.
Schizoaffective Disorder: Schizoaffective disorder may have a slightly better prognosis in some cases. This is particularly true when mood symptoms are well-managed with treatment. Effective treatment for mood disturbances can contribute to improved functioning and a more stable quality of life compared to schizophrenia.
Living With Schizophrenia and Schizoaffective Disorder
While schizophrenia and schizoaffective disorder share some similarities, the day-to-day challenges can look very different.
Schizophrenia
People with schizophrenia often experience:
- Disorganized thinking
- Hallucinations
- Delusions
These symptoms can make it hard to:
- Maintain a job
- Manage relationships
- Handle basic self-care like cooking or hygiene
Social withdrawal is common due to cognitive impairments or paranoia. How well someone functions often depends on the severity of their symptoms and the support they receive.
Schizoaffective Disorder
Schizoaffective disorder includes psychotic symptoms like schizophrenia but with added mood symptoms such as:
- Depression: low energy, lack of motivation, difficulty keeping up with responsibilities
- Mania: impulsivity, risky decisions, or strained relationships
Unlike schizophrenia, the mood symptoms in schizoaffective disorder can sometimes make the person seem more emotional or engaged.
However, the combination of mood instability and psychotic symptoms creates its challenges.
Key Differences in Functioning
- People with schizophrenia may face more consistent cognitive and social impairments, often requiring long-term support.
- Those with schizoaffective disorder might have periods of better functioning because mood symptoms can be episodic. However, mood instability adds complexity to daily life.
Understanding these differences can help caregivers, loved ones, and professionals provide tailored support. Both conditions benefit from early intervention and ongoing treatment, but the unique patterns of symptoms mean individuals need different strategies to navigate daily life successfully.
Challenges in Diagnosis and Misdiagnosis
Diagnosing mental health conditions can be incredibly challenging due to the significant overlap of symptoms across different disorders.
For example, symptoms like fatigue, irritability, or difficulty concentrating may be present in conditions such as anxiety, depression, or ADHD, making it difficult to pinpoint the exact issue without thorough evaluation.
These complexities often lead to delayed diagnosis or even misdiagnosis, which can impact the effectiveness of treatment and the overall well-being of the individual.
Mental health professionals play a critical role in navigating these challenges by utilizing tools such as the DSM-5 criteria to conduct a detailed differential diagnosis. This involves carefully distinguishing one mental health condition from another by analyzing symptom patterns, medical history, and other contributing factors.
Accurate diagnosis is essential for tailoring the right treatment plan and ensuring that individuals receive the support they need. Raising awareness about these challenges is key to improving diagnostic accuracy and fostering a better understanding of mental health among both professionals and the general public.

Real-Life Case Studies
Case Study 1: Living with Schizophrenia
John, a 28-year-old software developer, began experiencing auditory hallucinations and believing he was being surveilled during his college years. His symptoms grew more severe, leading to difficulties at work and withdrawing from friends. After diagnosis and starting treatment—antipsychotic medication combined with therapy—John began to rebuild his life. Today, he uses strategies learned in therapy to manage stress and prevent symptom relapse.
Case Study 2: Managing Schizoaffective Disorder
Anna, a 35-year-old graphic designer, struggled with extreme mood swings coupled with periods of psychosis. She recalls manic episodes when she spoke rapidly and felt invincible, followed by depressive episodes where even getting out of bed felt impossible. After her diagnosis, Anna started a personalized treatment plan that included antipsychotic medication, mood stabilizers, and ongoing therapy. She credits early intervention and family support for helping her find stability and thrive in her career.
Comparing Their Experiences
While both John and Anna faced psychosis, Anna’s mood swings significantly shaped her experience. This underlines the importance of precise diagnosis in tailoring effective treatment options.
Schizoaffective disorder vs Schizophrenia FAQ
What are the symptoms of schizophrenia vs. schizoaffective disorder?
Schizophrenia primarily involves symptoms like hallucinations, delusions, disorganized thinking, and cognitive impairments. Schizoaffective disorder includes these symptoms but also features significant mood episodes, such as depression or mania, making it a combination of schizophrenia and mood disorder symptoms.
How is schizoaffective disorder different from schizophrenia?
The key difference is the presence of mood episodes in schizoaffective disorder. While schizophrenia focuses on psychosis and cognitive issues, schizoaffective disorder combines these with periods of significant mood disturbances, like depressive or manic episodes.
What are the best treatment options for schizophrenia and schizoaffective disorder?
Treatment for both conditions typically involves antipsychotic medications to manage psychosis. For schizoaffective disorder, additional treatments like mood stabilizers or antidepressants may be prescribed to address mood symptoms. Therapy, support groups, and psychosocial interventions are also vital for long-term management.
What is psychosis in schizophrenia and schizoaffective disorder?
Psychosis refers to losing touch with reality, which can include hallucinations (seeing or hearing things that aren’t there) and delusions (strong, false beliefs). Both schizophrenia and schizoaffective disorder involve psychosis, but schizoaffective disorder often occurs alongside mood episodes.
Can you have both schizophrenia and schizoaffective disorder?
No, you cannot have both conditions simultaneously. Schizoaffective disorder is a distinct diagnosis that includes both psychotic symptoms and mood disturbances. A proper diagnosis depends on the patterns and duration of symptoms observed.
The Path Forward
Whether living with schizophrenia or schizoaffective disorder, one thing is clear: early intervention and holistic treatment pave the way to stability and improved quality of life.
If you or a loved one are navigating these challenges, don’t hesitate to reach out to mental health professionals for guidance and support. You’re not alone.
For personalized support, consider talking to our Empathy Health Clinic professionals who specialize in these disorders.
Recovery is possible, one step at a time.
